iEDeX technology is currently deployed in three healthcare solution environments.

iEDeX MD is integrated with the physicians practice management software and fully automates query of patient eligibility information during the scheduling process. Eligibility response information is directly imported into HIS or EMR data fields and supports medicaid, medicare, and commercial health plans.
iEDeX Exchange is a resolution platform and provides a web-based transaction comparison tool allowing you and your vendor to share the same view of detailed exchanged transactions, in the same format.
iEDeX Enrollment is a solution designed specifically for the health plans to streamline their enrollment procedure. iEDeX™ Enrollment is a seamless solution that can be integrated with payors managed care information system to support automated enrollment processing.
Interoperability
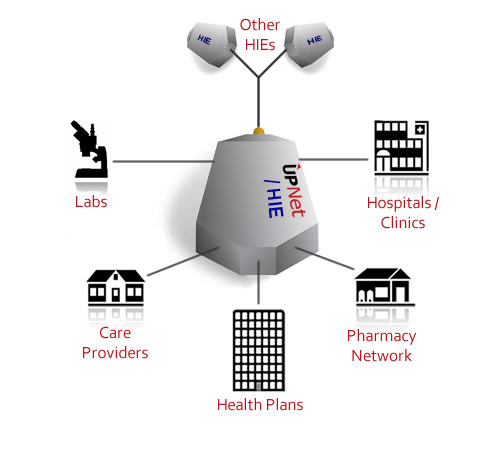
Information Technology is the driving force in the healthcare industry today. A growing need for on-demand access to medical information has prompted industry leaders to move towards a healthcare information exchange (HIE) based system, bringing together individual healthcare organization's data as one. The software applications designed for any particular healthcare service should be interoperable to facilitate the flow of information among the healthcare organizations and maintain a flawless communication among its various users.
Interoperability sets standardized rules of engagement between systems - for example, how medical information should be stored and communicated in the local network and how to interact with the HIE. Healthcare organizations with existing systems require a way to translate their data into these standardized types and check compliance to communicate effectively in local and wide-area networks.

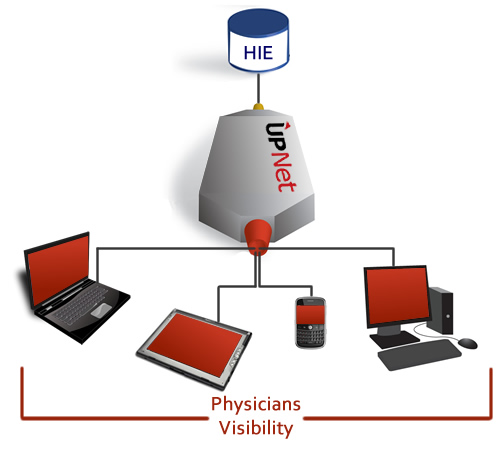
For physicians, interoperability allows more informed decisions to be made; for patients, it provides more personalized care and a more streamlined experience. For healthcare organizations as a whole, interoperability means more efficient use of IT and greater potential for future improvement.
Interoperability provides simple access to information at the point of care and enables communication of data across facilities, mobilizing the access points of essential patient data. It also aids in integrating software to healthcare information exchanges in order to grow IT capacity and functionality. Interoperability also directly affects the economy of healthcare markets. Due to the widespread recognition of IT in the healthcare industry, many competing products are being launched into the market. Interoperability of a product significantly promotes its brand name and ensures against potential market failure, in addition to upholding the quality of the product and maintaining consistency.
iEDeX Exchange
UpNet'siEDeX™ Exchange is a many-to-many transaction exchange engine. It enables participants to exchange Electronic Health Records (EHR) with any healthcare organization using the participants preferred structure, while facilitating the participant's compliance with HIE requirements.
iEDeX™ Exchange provides interoperability that maintains a smooth data flow across the entire network. Through enhanced visibility, data flows can be monitored and reported in real-time. As a resolution platform, a web-based transaction comparison tool is provided allowing you and other participants to share the same view of detailed exchanged transactions, in the same format. To be an effective information factory, transparency to consumers and participants (who have the proper credentials) is essential. iEDeX™ Exchange allows real-time or batch inquiries on various types of data (ranging from clinical data, eligibility data, claim data, administrative data to billing, etc) from multiple sources to streamline work flow process and provide analytical capabilities.
Why iEDeX™ Exchange?
iEDeX™ exchange is a many to many transaction exchange engine that supports interoperability by:
- Integrating and standardizing high volumes of data passing through multiple healthcare trading partners such as health plans, clearing houses, and benefit administrators
- Translating messages coming from trading partners in different formats like X12,HL7, XML, and proprietary format into a standard format that can be viewed online
- Supporting both batch based and real time responses
- The system can receive and display any or all of the HIPAA mandated ANSI ASC X12 transactions between healthcare trading partners
Features
- A many to many transaction exchange engine
- Participants can exchange data/documents with any trading partners, using participant preferred structure
- Web-based technology and low monthly fee structure
- Smooth data interchange due to interoperability
- Web-based transaction comparison tool allows you and your vendor to share the same view of detailed exchanged transactions, in the same format
- Utilizes encryption technology for data security
- Allows real time or batch inquiries on various type of data
- Allows participants to check claim status online
- Allows participants to sign up for direct deposits and payroll interface
- Maintains ease in the workflow process
iEDeX MD
A registrar is scheduling a patient by telephone while, in the background, the scheduling system verifies eligibility and determines benefit coverage for the requested appointment. Thus the registrar is able to inform the patient of payment up front.
A mirage? No longer.iEDeX™ MD is a seamless, integrated, eligibility and benefit verification solution that helps physician offices to confirm patient's insurance eligibility at the point of care. Historically verification was an expensive, costly, and impractical affair. The process typically involved web site look-up, fax or interactive voice response, or manually calling the health plan. iEDeX MD is integrated with the physicians practice management software and fully automates query of patient eligibility information during the scheduling process, removing the need to have someone manually query for the information.
- Insurance eligibility verification is among the fastest growing EDI transactions (health data management)
- Providers using EDI could reduce eligibility verification labor costs by up to 50% (CORE Patient Identification Survey)
- Health plans using EDI would also realize significant savings given that the average labor cost per call is $1.38 (CORE Patient Identification Survey)
- Stanford University reports that 50% of its bad debt was attributable to bad eligibility data
As a further testament to the benefits of electronic transactions, Milliman, Inc. compared differences in the cost of manual and electronic transactions for a typical physician practice environment. The greatest savings occurred for those transactions where technology eliminates telephone time, such as eligibility verification and claim status checks, for which electronic transactions resulted in 80% to 90% cost reductions! (Electronic Transaction Savings Opportunities For Physician Practices, Milliman Inc.)
Features
- Eligibility inquiry is automatically generated from physician's appointment scheduling system
- Eligibility response information is directly imported into HIS or EMR data fields
- Immediate/real-time response
- Supports medicaid, medicare, and commercial health plans
- Permits user to perform inquiries on demand or in an automated fashion
Provides real-time information regarding:
- Whether the health plan covers the patient
- Whether the service to be rendered is a covered benefit (including co-pays, coinsurance levels, and base deductible levels as defined in member contract)
- What amount the patient owes for the service
- What amount the health plan will pay for authorized services
- Coordination of Benefits (COB) information
Functional Values
- CORE certified
- HIPAA compliant
- Ability to retrieve eligibility and benefits information via multiple search criteria
- Provision to print the eligibility response
- Automated, easy to use system requiring little manual intervention
- Compatible with all major Health Information System (HIS) and Electronic medical Record (EMR) platforms
- Ensures patient privacy by using encryption and security technology
- Requires minimal IT staff time and system resources to install / maintain
- 24/7 customer service
Provider Values
- Provides real time access to eligibility data either by individual or batch
- Saves time by replacing telephone intensive eligibility inquiries
- Streamlines the electronic medical claim submission by ensuring that claims are submitted to the correct payer in a timely manner
- Reduces bad debt / risk
- Accelerates cash flow
- Reduce / reallocate staff by removing manual processes
- Ability to identify excluded benefits and determine benefits requiring pre-certification
- Provides more detailed eligibility information than telephone responses
Patient Values
- Improved customer service as staff can provide information to patients about their coverage and benefits
- Confirm patient eligibility prior to office visit
- Accurate identification of patient's financial responsibilities
iEDeX Enrollment
- More than 250 million Americans are enrolled in health insurance plans.
- Many other states are working to identify opportunities to expand state-funded health care coverage.
- The benefit enrollment and maintenance 834 is becoming the standard of choice for the Human Resource Department.
- The state of MA passed a law requiring all residents to obtain health insurance.
iEDeX Enrollment leverages the power of technology to automate your enrollment process. It is a solution designed specifically for the health plans to streamline their enrollment procedure.iEDeX™enrollment is a seamless solution that can be integrated with your managed care information system to support automated enrollment processing.
iEDeX enrollment automatically examines inbound enrollment files to ensure that they meet 834 EDI industry standards. Standard documents are integrated into the payers proprietary managed care information system while erroneous documents are queued up for correction by internal IT staff.
In addition, the system provides an option to the employer to self correct erroneous data by generating and sending error alert emails to employers. Employers are provided web-portal access to correct errors and enroll new employees. The system has an intuitive user-interface for upfront correction of enrollment documents that don't meet EDI standards.
Why iEDeX™ Enrollment?
- Employees who are satisfied with their employer's health plan communication are 5 times more likely to be satisfied with their health plan than employees who are not satisfied with their communications. (Watson Wyatt)
- Self service open enrollment reduces inquiries by 75%. (Hunter Group).
- 95% of HR and benefit managers consider automated enrollment, administration, communication, and supplier management of benefit programs a technology imperative. (RewardsPlus).
- Using ANSI 834 standard for linking employer and payor networks to exchange enrollment information is estimated to save employers with 50 employees or more $2.0 to $4.1 billion per year (net of transaction costs), and save payors $110 to $220 million net per year (Workgroup for Electronic Data Interchange).
- AT&T saved $15 million in first year of EDI enrollment and reported substantial decrease in claims paid to ineligible claimants (Healthcare Financial Management).
- Regents of the University of California implemented HIPAA compliant enrollment that found and corrected $1million billing error (McLure-Moynihan Inc.).
- Extensive, on-going communication among constituents is critical to the success of EDI implementation (Workgroup for Electronic Data Interchange).
Features
- Ability to handle multiple product types for multiple payers.
- Produces real-time quotes for different health insurance plans.
- Accepts enrollment documents in employers proprietary formats.
- Automatically enroll new members using information on paper or electronic forms.
- Generates HIPAA complaint enrollment files in 834 standard.
- Integrates the new member enrollment information to payers proprietary managed care information system.
- Can be integrated with health plan's claims and billing system.
- 24/7 customer support.
Values
- Eliminates the cost and time associated with paper intensive enrollment procedures.
- Reduction in errors associated with manual enrollment.
- State of the art technology that identifies and alerts about error trends.
Improve employer/sponsor relations
- Eliminates the errors and time-lags in benefit administration.
- Reduces costs associated with claim rejections.
- Upfront correction of new member enrollment data.
- Empowers employers by providing them with web-portal access to self-correct enrollment errors.
- Pro-actively market superior administrative capabilities to prospective and current employer groups.
Improve enrollee relations
- Lower claims expense and improved customer service.
Strengthen provider relations
- Minimize claim rejection rates.
- Expedite transaction processing cycles.
- Increase auto-adjudication rates by identifying and correcting enrollment errors.